Keeping Vaccines At The Correct Temperature.
Introduction
Vaccines are biological substances that may lose their effectiveness quickly if they become too hot or too cold at any time, especially during transport and storage. Vaccines and other medical substances such as blood products etc. naturally biodegrade over time, and storage outside of the recommended temperature range – including during transport and storage – may speed up loss of potency, which cannot be reversed. This may result in the failure of the vaccine to protect, as well as resulting in vaccine wastage. It is essential that all those handling vaccines follow policies to ensure cold chain compliance.
Vaccines therefore need to be stored at their correct temperatures and, not only that, but an inviolate record needs to be maintained to prove that the correct storage temperatures have been maintained. Different vaccines need to be stored at different temperatures for example the Astra-Zeneca Covid-19 vaccine needs to be stored at between 2 and 8˚C as are most vaccines, however the Pfizer-BioNTech COVID-19 vaccine must be stored in an ultra-cold freezer that will holds the vaccine between -90°C and -60°C. Whatever the vaccine, they must be stored at the correct temperature and an inviolate record maintained in order to ensure the safety and efficacy of the product.
Unless specific advice states otherwise, including manufacturer’s stability data, vaccines that have not been stored correctly are therefore no longer within the terms of the marketing authorisation and should not be used.
There are a number of published documents that give guidance to best practice, and we have particularly drawn on two as detailed in the references.
The World Health Organisation has also made recommendations on vaccine storage and transportation so that an efficient ‘cold chain’ is established, that ensures correct temperatures are maintained and vaccine potency assured (WHO, 2006).
These SOPs should include details of the designated staff member (named responsible person) and the deputy staff who covers in their absence - a minimum of two people
Vaccine Storage
Examples of good practice include:
aiming for +5°C, the midpoint in the +2°C to +8°C range designating areas within the refrigerator for different vaccines so that all staff know where specific vaccines are stored. Glass doors or labels on the outside of fridges can reduce the time the door needs to be open, and rotating vaccine stocks within the refrigerator so that those with shorter expiry dates are at the front and used first
Vaccines should only be stored in PHARMACEUTICAL FRIDGES and ONLY vaccines should be stored in this fridge.
Domestic fridges should NOT be used for vaccine storage.
Pharmaceutical fridges should have at least the following specifications or features:
- Either solid or glass door which is lockable. All vaccines are Prescription Only Medicines (POMs) and must be stored under locked conditions.
- Capable of maintaining an internal air temperature between +2°C and +8°C and the temperature can be read externally.
- Ice must not build up in the fridge therefore it is recommended that all fridges have fully automatic defrosting. If defrosting is necessary, vaccines should be stored temporarily in a suitable alternative refrigerator or in a validated medical-grade cool box, but for the minimum possible time
- Fan operated, forced air cooling for temperature stability.
- Integral controller enabling staff to set the required temperature and easily monitor and record current /minimum / maximum levels.
- Both audio and visual alarm signal when a temperature deviation lasts for more than 15 minutes.
- Open door sensor which alerts the user that the fridge door is not properly closed and sealed.
- Large enough to hold 6 weeks inventory. And there is sufficient space around the vaccine packages for air to circulate and there is sufficient capacity for vaccines for seasonal/ additional programmes such as the annual influenza vaccination campaign
- All fridges must have a unique identifier, such as a serial number.
- The refrigerator must be safe, for example by undertaking regular visual inspections and portable appliance testing (PAT). (The Electricity at Work Regulations (1989) require electrical systems to be ‘maintained’.)
- Fridges must be maintained in a clean condition and a maintenance contract that allows for at least yearly servicing and calibration of the temperature sensors must be in place and records maintained
- Steps must be taken to reduce the probability of accidental interruption of electricity supply, such as installing a switchless socket or clearly labelling the vaccine refrigerator plug.
Fridge Monitoring
The temperature conditions within all Pharmaceutical Fridges must be monitored on a regular basis to ensure that the vaccines are maintained within their recommended limits and an inviolate record maintained. This can be done by a nominated individual physically recording the current, maximum, and minimum temperatures as least twice a day. However, relying on an operative has inherent risks and the temperatures are only noted retrospectively when it is too late to take appropriate action. A much better solution is to use an Alarming Data Logger such as the Cadmus CTX series from Signatrol which provides all the necessary requirements for data logging and alarming.
When a new pharmaceutical fridge is installed in its permanent position or when a fridge is moved, it should be allowed to stand for minimum of 24 hours before it is switched on. This allows gases to reach equilibrium before power is switched on. Then record the temperature for 48 hours to ensure it is maintaining the correct temperature.
If the vaccine fridge has been repaired the temperature must be monitored for at least 48 hours before using the fridge to store a new supply of vaccines.
Monitoring and Alarming
All refrigerators should be monitored using a system that is separate from the fridge control circuitry. Temperatures (current Max and Min) in the refrigerator must be monitored and recorded at least once each working day and documented on a chart for recording temperatures.

Cadmus Alarming Data Logger from Signatrol
Data loggers, that provide a continuous record of temperatures within the fridge, are recommended. The calibration of thermometers/loggers should be checked annually to ensure that they are working correctly. The records should be readily accessible for easy reference and retained until the next audit. Refrigerator failure or disruption of the cold chain Arrangements should be in place for back-up facilities to be available in the event of the refrigerator failing or breaking down.
The best and most cost-effective method available to monitor temperatures is by using an appropriate data logger.’ An appropriate Data Logger should have the following attributes:
- A data logger (a battery powered continuous temperature recording device) should be used in fridges where vaccines are stored. The sensor should be placed in the middle of the fridge adjacent to the vaccines.
- This device must be independent of the fridge and continue to record the temperatures even when there is no power supply and therefore gives an accurate account of the temperatures reached and the duration of any temperature breach.
- Data loggers should be set to record temperatures at 5 to 10 minutes intervals.
- The data logger should be downloaded and reviewed regularly (at least once every two weeks), and the electronic or printed record should be retained indefinitely. The stored data will suffice as a permanent temperature record for the fridge.
- Once a temperature breach is registered by fridge thermometer or the fridge has alarmed, the data should be downloaded to confirm the temperatures reached and the duration of the breach.
- The data should be stored in encrypted form which cannot be altered by ordinary means.
The CTX series of data loggers from Signatrol provide the facility to record the temperatures at two points, to generate audio and visual local alarms and to send email messages to a number of different contacts (using their unique Shift Planner feature) and monitors door open/closed status.
Cost Saving
When you employ someone to record manual readings (or in fact several people to cover shift patterns, holidays etc.) you have an inherent cost, the employment cost of the person and management costs.
In addition, you must manage the system i.e., ensure that the responsible person is in fact in work and that they did not forget to take the readings, and that the readings are correct and legible etc. This has a direct cost in salaries and an indirect cost in that readings are only taken in retrospect so that if there was a problem it is too late to take corrective action.
Signatrol’s CTX series data loggers seamlessly record all relevant temperatures under the control of the Administrator (responsible person) Because the loggers can accept two external temperature probes, they can be used to detect a problem early enough to be able to take corrective action and hence avoiding the need to destroy the vaccines.
By using an Alarming Data Logger such as Signatrol’s CTX series, which can accept two remote sensors, the system can be set up to provide advanced warning enabling corrective action to be taken before the problem affects the actual vaccine being stored.
The way this is done is using Load Bottles.

Load bottles are available to accurately mirror the response time of the vaccines. There are therefore two sensors placed in the fridge.
The load bottle is normally used in conjunction with the second temperature sensor. The first sensor can be used to monitor the air temperature within a fridge/freezer to provide immediate notification of a potential failure, and the second external sensor, placed inside the bottle to represent the actual product.
The fridge sensor can raise an alarm as the temperature in the fridge rises, due to a malfunction for example, before the temperature in the stored product goes outside its recommended range. In this way the fridge malfunction can be addressed, and the vaccine moved to a correct storage environment before any damage is done. Thanks to this early alarming technique, one of our customers has prevented the scrapping of over £200,000 worth of vaccines.
Security & Compliance
Any data stored must be secure, inviolate, stored indefinitely for easy access by authorised people. The system should use an Administrator / User model whereby the Administrator (often called the Responsible Person) effectively ‘owns’ the system, adds and suspends users and decides how much or how little the user can interact with the system.
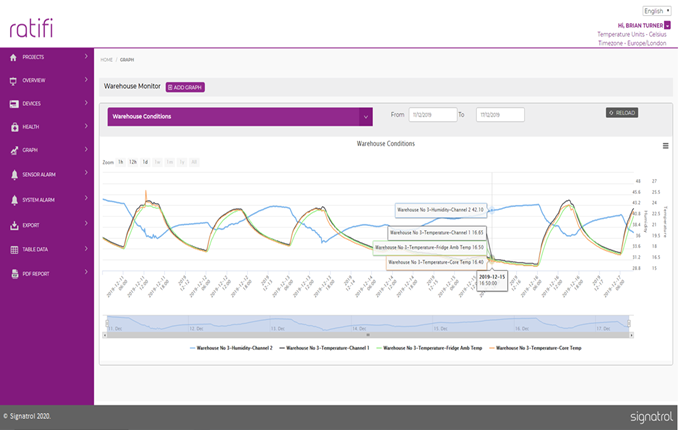
The CTX system stores all data on the Ratifi Cloud software in encrypted form and also supports Enterprise Security to prevent unauthorised hacking into the local WIFI network.
The Ratifi system allows you to do the following:
- Print or export your results in PDF or CSV formats
- Automate your reports and send to multiple addresses (Essential to any 21 CFR Part 11 validation system.
- The Cloud based system allows the Administrator to configure the system to their requirements.
- The system records any changes with Dates and Times, which may have made e.g., changes to users, locations, and account settings etc. for subsequent retrieval during the audits
- Provides an easily retrievable Audit Trail
- Through the Cloud, automated reports can be set up remotely providing daily, weekly, and monthly reports and can then be sent to multiple email addresses. This becomes vital when considering your regulatory compliance and auditable requirements.

Vaccine Transport
Vaccines must be transported in such a way as to maintain their temperatures within their recommended range.
The temperature on delivery should be checked and recorded to show that vaccines were in temperature on delivery. Vaccines are normally transported in either appropriate refrigerated containers or Validated Cool Boxes.
Refrigerated Containers:
Vaccine boxes must not touch the sides, back or bottom of the fridge. Air needs to circulate therefore the fridge should not be overfilled, as this will prevent proper airflow. Ideally, the fridge should never be more than two thirds full.
Validated cool boxes:
Domestic cool boxes should not be used to store, distribute, or transport vaccines. Validated cool boxes and cool packs from a recognised medical supply company should be used in conjunction with validated maximum– minimum thermometers or approved Data Loggers. Cool packs should be stored in accordance with the manufacturer’s instructions, usually at +2˚C to +8˚C (not a freezer compartment) to ensure they maintain the cold chain at the right temperature. In general, ice packs and frozen cool packs should not be used as there is a danger of these freezing some vaccine doses during transit. The exception to this is when the cool box manufacturer’s instructions specifically state that ice packs should be used. Individual manufacturer’s instructions should be strictly adhered to.
A validated cool box provides ongoing assurance that the vaccines will be maintained within the cold chain temperature range during transport. With time and use, cool boxes may no longer be able to maintain this temperature range for extended periods, so monitoring is always required. The cool box manufacturer should also provide sufficient evidence for assurance that a stable temperature within the range of the cold chain can be maintained for several hours.
Vaccines must be kept in the original packaging, wrapped in bubble wrap (or similar insulation material), and placed into a cool box with cool packs as per the manufacturer’s instructions. This will prevent direct contact between the vaccine and the cool packs and will protect the vaccine from any damage.
When transporting vaccines, the named individuals are responsible for ensuring that only the amounts of vaccines necessary for each session are removed from the vaccine refrigerator. These should be placed quickly into the validated cool boxes and opening must be kept to a minimum. If there are any unused vaccines left over at the end of a vaccination session, providing there is evidence from the temperature monitoring that the cold chain has been maintained, the vaccines can be returned to the vaccine refrigerator. Returned vaccines should be used at the earliest opportunity. If the cold chain cannot be guaranteed, a risk assessment should be done.
On arrival, vaccines must be placed immediately in the vaccine fridge and must never be left at room temperature.
Signatrol have a range of portable data loggers (SL50 series, Tempmate etc) Than can be placed with the vaccines to ensure that they have been maintained at the correct temperatures. We believe that this is the only way it you can be absolutely sure that this was the case during the entire journey.
Monitoring, Audit and Evaluation
Audits on all pharmaceutical fridges that are used for storing vaccines, should be completed annually unless issues identified require earlier repeat audits.
A record of this audit should be kept. Other sites that have been involved in a cold chain failure will be selected randomly and re-audited.
References
- HSE Guidelines for maintenance of cold chain in vaccine fridges
and management of vaccine stock
Document reference number NIO-01
- Green Book Chapter 3 v2_1
Storage, distribution, and disposal of vaccines
